User:Karsten Theis/Insulin
From Proteopedia
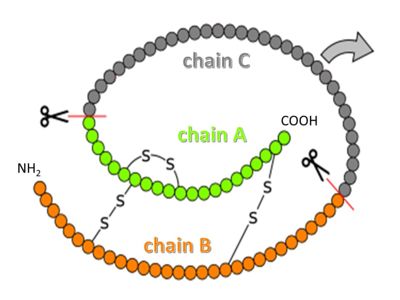
Insulin is a peptide hormone that helps to maintain blood sugar within a healthy range by regulating carbohydrate and lipid metabolism throughout the body[1][2]. It is secreted by specialized cells in the pancreas and acts by binding to insulin receptors on other cells. Insulin in its mature form contains two peptide chains connected by disulfide crosslinks, and occurs either as monomer or as hexamer. Administering insulin in carefully determined doses at the appropriate times is used in managing diabetes, a chronic condition where the body fails to maintain blood sugar levels by itself.
Contents |
Function
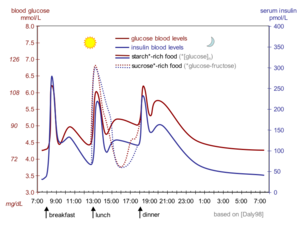
Our blood sugar level (i.e. glucose concentration) varies over time with food intake and exercise, but has to remain in a narrow range so we stay healthy (not become hyperglycemic or hypoglycemic). Insulin, together with glucagon, regulates blood sugar levels by changing fuel metabolism in all cells [3] on a timescale of minutes and hours. In simplest terms, the presence of insulin in the blood signals the well-fed stage, while the presence of glucagon signals the fasting stage.
Biosynthesis and processing of insulin occurs in the beta cells of the pancreas. The beta cells are found in the islets of Langerhans, which also contain the alpha cells that synthesize glucagon. Insulin is made as a 110 amino acid pre-proinsulin, which is processed to the mature 51 amino acid insulin and targeted to secretory vesicles. In a healthy adult, about 200 units of insulin are available in the pancreas, of which 30-50 units are secreted daily[4]. With a unit of insulin corresponding to 0.0347 mg mature insulin [5], the body contains only about 7 mg of insulin. In its stored form, insulin is a hexamer complexed to zinc ions.
Insulin is constantly released into the blood stream at a basal level. When blood glucose levels rise after a meal containing carbohydrates (sugars and starches), increased intracellular glucose in the beta cells triggers a series of processes that change the intracellular calcium concentration. First, the calcium concentration rises and stays elevated for 5-10 minutes, and then it spikes in intervals of roughly 3 minutes. Whenever calcium concentrations are high, insulin-containing vesicles merge with the plasma membrane, releasing insulin into the blood stream in the same temporal pattern as the calcium spikes[6]. The insulin is released into the bloodstream, where it first reaches the liver via the portal vein[7], and then the other organs after insulin-containing blood returns from the heart.
Once insulin binds to its receptor, the receptor is removed from the plasma membrane, insulin is degraded and the receptor is recycled[10]. The majority of insulin is removed from the bloodstream this way on its first pass through the liver. The half-life of insulin in the blood plasma is about about 4-6 minutes[11].
Disease and Treatment
In patients with diabetes, insulin signalling is compromised[12]. In type I diabetes, insulin is not produced sufficiently because the beta cells in the pancreas are absent or compromised by an autoimmune event. The onset of type 1 diabetes is rapid, and often occurs early in life ("juvenile diabetes"). In type II diabetes, insulin is secreted at normal or even elevated levels, but the target cells do not respond properly, for reasons not yet understood[13]. The onset of type 2 diabetes is gradual (over years), and there are warning signs (like insulin resistance) that in some cases helps to avert the onset by certain changes in lifestyle and diet[14].
Type 1 diabetes is managed by administering insulin. The challenge is to keep the blood sugar level in a healthy range while conditions change (food intake, exercise, illness). Insulin can not be given orally because it is broken down in the digestive tract. Instead, it is administered via subcutaneous depots or in other non-oral forms). There are long-acting and short-acting preparations of insulin to provide the basal level and to manage spikes in blood glucose levels, respectively. Type 2 diabetes is managed in a variety of ways, which may include administration of extra insulin to partially counteract the diminished signalling capacity.
Structure
| |||||||||||
References
- ↑ Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. PMID:10927996
- ↑ Weiss MA, Lawrence MC. A thing of beauty: Structure and function of insulin's "aromatic triplet". Diabetes Obes Metab. 2018 Sep;20 Suppl 2:51-63. doi: 10.1111/dom.13402. PMID:30230175 doi:http://dx.doi.org/10.1111/dom.13402
- ↑ https://www.yourhormones.info/hormones/insulin/
- ↑ https://www.britannica.com/science/insulin
- ↑ https://www.who.int/biologicals/expert_committee/BS_2143_Human_Recombinant_Insulin_final.pdf
- ↑ Henquin JC. Regulation of insulin secretion: a matter of phase control and amplitude modulation. Diabetologia. 2009 May;52(5):739-51. doi: 10.1007/s00125-009-1314-y. Epub 2009, Mar 14. PMID:19288076 doi:http://dx.doi.org/10.1007/s00125-009-1314-y
- ↑ "https://www.diabetesselfmanagement.com/diabetes-resources/definitions/portal-vein/"
- ↑ https://pdb101.rcsb.org/motm/182
- ↑ 9.0 9.1 Gutmann T, Kim KH, Grzybek M, Walz T, Coskun U. Visualization of ligand-induced transmembrane signaling in the full-length human insulin receptor. J Cell Biol. 2018 May 7;217(5):1643-1649. doi: 10.1083/jcb.201711047. Epub 2018, Feb 16. PMID:29453311 doi:http://dx.doi.org/10.1083/jcb.201711047
- ↑ Haeusler RA, McGraw TE, Accili D. Biochemical and cellular properties of insulin receptor signalling. Nat Rev Mol Cell Biol. 2018 Jan;19(1):31-44. doi: 10.1038/nrm.2017.89. Epub 2017 , Oct 4. PMID:28974775 doi:http://dx.doi.org/10.1038/nrm.2017.89
- ↑ Duckworth WC, Bennett RG, Hamel FG. Insulin degradation: progress and potential. Endocr Rev. 1998 Oct;19(5):608-24. doi: 10.1210/edrv.19.5.0349. PMID:9793760 doi:http://dx.doi.org/10.1210/edrv.19.5.0349
- ↑ https://www.endotext.org/section/diabetes/
- ↑ Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016 Jan;126(1):12-22. doi: 10.1172/JCI77812. Epub 2016 Jan 4. PMID:26727229 doi:http://dx.doi.org/10.1172/JCI77812
- ↑ doi: https://dx.doi.org/10.1530/endoabs.56.PL5
- ↑ Davidson HW. (Pro)Insulin processing: a historical perspective. Cell Biochem Biophys. 2004;40(3 Suppl):143-58. PMID:15289650
- ↑ doi: https://dx.doi.org/10.1101/679233
- ↑ Scapin G, Dandey VP, Zhang Z, Prosise W, Hruza A, Kelly T, Mayhood T, Strickland C, Potter CS, Carragher B. Structure of the Insulin Receptor-Insulin Complex by Single Particle CryoEM analysis. Nature. 2018 Feb 28. pii: nature26153. doi: 10.1038/nature26153. PMID:29512653 doi:http://dx.doi.org/10.1038/nature26153